Could you be a candidate for bariatric surgery? Take this quiz to find out →
Paul D. Bailey, III, MD
BLOG
Patient Resources
Risks and Complications: Understanding the Potential Side Effects of Bariatric Surgery
Bariatric surgery, an effective weight loss solution, comes with various potential risks and complications that are important to understand:
Short-term Risks: These include surgical complications like excessive bleeding, anesthesia reactions, blood clots, and post-operative risks such as infections and leaks at surgical sites. Thankfully, surgical complications following bariatric surgery are rare but occur even at large centers and with experienced surgeons. Quick recognition of problems and proper management are essential to minimize complications from these issues. Nausea and dehydration can occur with any stomach surgery and must be watched for closely in the first days to weeks after surgery.
Long-term Complications: Patients may face nutritional deficiencies, gastrointestinal issues like acid reflux and ulcers, dumping syndrome, gallstones, and potential mental health impacts like depression or anxiety.
Additional Concerns: There's a risk of weight regain if lifestyle and dietary changes are not maintained, and significant weight loss can result in excess loose skin, possibly requiring further surgery.
Informed Consent: It's crucial for patients to discuss all potential risks and benefits with healthcare providers and understand the long-term commitment, including lifestyle changes and regular medical follow-up. You should be fully informed of all issues and have any questions or concerns addressed by your surgeon before surgery.
Lifelong Commitment: Bariatric surgery is not a guaranteed permanent solution and requires a lifelong commitment to achieve and maintain its benefits.
Candidates for bariatric surgery are typically selected based on several key criteria:
Body Mass Index (BMI): Usually, candidates have a BMI of 40 or higher, or a BMI of 35-39.9 with serious weight-related health issues. Recent recommendations from the ASMBS have lowered this threshold and are starting to be recognized by hospital systems and insurance providers.
Previous Weight Loss Efforts: Candidates should have attempted weight loss through diet and exercise without long-term success.
Health Status: A comprehensive health evaluation is required to assess any obesity-related conditions and overall suitability for surgery.
Psychological Evaluation: Mental preparedness and stability are assessed to ensure candidates can handle the surgery and its aftermath. Depression and eating disorders should not prevent someone from having surgery but need to be controlled preoperatively.
Understanding and Commitment: Candidates must understand the risks of the surgery, commit to lifestyle changes, and follow-up care.
Age: While primarily adults are considered, in some cases, adolescents with severe obesity-related health problems may qualify.
These criteria ensure that the surgery is both safe and likely to be effective for the patient. Each candidate undergoes a thorough evaluation to determine their suitability for bariatric surgery.
Understanding the Risks and Complications
Any bariatric surgery is a significant medical procedure with various risks and potential complications:
Common Risks:
Infections: Possible at the incision site or internally.
Blood Clots: Increased risk of deep vein thrombosis and pulmonary embolism.
Nutritional Deficiencies: Due to decreased food intake and/or changes in absorption, requiring lifelong supplementation.
Gastrointestinal Issues: Such as acid reflux, nausea, vomiting, and food intolerances.
Dumping Syndrome: Causing symptoms like nausea, light-headedness, feeling unwell, and diarrhea after eating certain foods.
Gallstones: Can develop due to rapid weight loss.
Psychological Effects: Including depression, anxiety, or body image issues.
Weight Regain: Possible if lifestyle changes are not maintained.
Rare but Severe Complications:
Anastomotic Leakage: A life-threatening leak from the surgical site.
Bowel Obstruction: Caused by scar tissue inside the abdomen or spaces created and not closed correctly after surgery.
Hernias: At the incision sites, potentially requiring more surgery.
Ulcers: Particularly in gastric bypass patients.
Stricture: A tightening in the gastrointestinal tract that limits how much food can pass through.
Severe Malnutrition: In extreme cases, due to altered digestion and poor intake.
Wernicke-Korsakoff Syndrome: Brain damage from thiamine deficiency.
Internal Bleeding: A rare post-surgery risk.
Factors Influencing the Risk of Complications
The risk of complications from bariatric surgery is influenced by several factors:
Pre-Existing Health Conditions: Conditions like diabetes, heart disease, and high blood pressure can increase risks for any surgery. Many patients who were not initially considered for bariatric surgery due to preexisting medical issues are now eligible for surgery as studies have shown they still see significant benefit from surgery although these conditions may increase the risk of surgical complications.
Patient's Age: There is no longer an age cutoff for surgery as older patients have been shown to have significant reduction in comorbidities as well as increased life expectancy and quality of life with surgery. Still, older patients may face higher risks due to decreased physiological resilience and the presence of more medical problems before surgery.
Body Mass Index (BMI): Higher BMI levels can lead to increased surgical and postoperative complications.
Nutritional Status: Pre-surgery nutritional deficiencies or poor diets can heighten post-surgical risks.
Lifestyle Factors: Smoking and alcohol consumption can adversely affect recovery and increase risks for severe complications.
Mental health issues or lack of readiness for post-surgery lifestyle changes can impact outcomes.
Type of Surgical Procedure: Different procedures come with varying levels of risk; more complex surgeries may have higher complication rates.
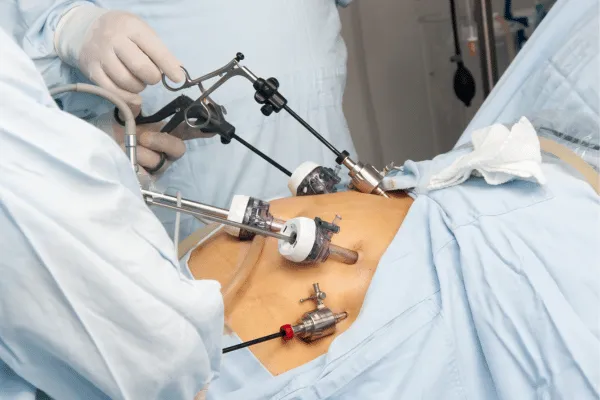
Surgical Technique and Experience: The surgeon's expertise and the chosen surgical method (e.g., robotic vs. laparoscopic vs. open surgery) significantly influence risk levels.
Postoperative Care: Quality postoperative care and adherence to follow-up protocols are crucial for minimizing complications and achieving the best outcomes.
Patient Compliance: Following recommended lifestyle changes, diet, and medication regimens is essential to reduce risks.
Understanding and managing these factors are key to minimizing complications and ensuring a safer surgical outcome.
The Importance of a Realistic Outlook
The success of bariatric surgery extends beyond the operating room, heavily reliant on patients having realistic expectations and committing to significant lifestyle changes post-surgery.
Realistic Expectations of Surgery Outcomes:
Weight Loss is Gradual: Patients need to understand that weight loss will not be instantaneous. It's a gradual process that occurs over several months to a couple of years.
Varied Individual Results: Weight loss and health improvements vary from person to person. Factors like pre-surgery weight, adherence to dietary guidelines, and exercise play a significant role.
Not a Standalone Solution: Surgery is a tool, not a cure for obesity. Long-term success depends on using this tool effectively in conjunction with lifestyle modifications.
Possible Need for Additional Surgeries: Some patients may require additional surgeries, such as for excess skin removal, depending on the amount of weight lost or surgery for reflux.
Commitment to Lifestyle Changes:
Dietary Modifications: Post-surgery, patients must adhere to a strict diet starting with liquids and gradually moving to solid foods. Long-term, a balanced, nutrient-rich diet in smaller portions is vital.
Regular Exercise: Incorporating regular physical activity is crucial for maintaining weight loss and overall health and wellbeing.
Ongoing Medical Follow-up: Regular check-ups, nutritional counseling, and monitoring for potential complications are essential aspects of post-surgery care.
Supplementation: Lifelong vitamin and mineral supplementation is necessary due to decreased food intake and altered nutrient absorption post-surgery.
Psychological Adjustment: Patients may need counseling to adapt to their changing body image and lifestyle. Support groups or therapy can be beneficial.
Avoidance of Unhealthy Habits: It’s important to avoid old habits that contributed to obesity, such as emotional eating, a sedentary lifestyle, smoking, or excessive alcohol consumption.
The Role of Informed Consent
Informed consent in the context of bariatric surgery is a critical process that ensures patients understand the full scope of the procedure, including its risks, benefits, and potential outcomes. This concept is not just a formal legal requirement but a fundamental aspect of ethical medical practice, especially for surgeries like bariatric procedures that have significant lifestyle implications.

Key Aspects of Informed Consent in Bariatric Surgery:
Comprehensive Information: Patients must receive detailed information about the surgery they are considering. This includes an explanation of the procedure, the type of bariatric surgery being recommended (e.g., gastric bypass, sleeve gastrectomy), and what the surgery entails.
Understanding Risks and Benefits: The surgeon should explain both the potential benefits (such as weight loss, improvement in obesity-related conditions) and risks (including short-term surgical risks and long-term lifestyle changes and complications).
Post-Surgical Lifestyle Changes: Patients should be informed about the necessary post-operative lifestyle changes, including diet, exercise, and follow-up medical appointments, and how these changes are essential for the success of the surgery.
Potential for Further Surgery: In some cases, additional surgeries (like for excess skin removal) may be necessary, and patients should be aware of this possibility.
Alternative Options: Patients should be informed about alternative weight loss methods and why surgery may be the recommended option.
Realistic Expectations: Setting realistic expectations regarding weight loss goals, changes in body image, and overall health improvements is a key part of informed consent.
Opportunity for Questions: Patients should have the opportunity to ask questions and express concerns, ensuring they fully understand what the surgery entails.
Importance of Informed Consent:
Autonomy and Decision-Making: Informed consent respects the patient's autonomy, allowing them to make an educated decision about their health and body based on a full understanding of the implications. You have the ultimate say in what is done for you.
Preparation for Post-Surgery Life: Understanding the full scope of what the surgery entails, including the commitment to lifestyle changes, prepares patients mentally and emotionally, which is crucial for post-surgery success.
Building Trust: This process helps in establishing trust between the patient and the healthcare team, as it demonstrates transparency and honesty regarding the procedure.
Deciding on bariatric surgery requires careful evaluation and consultation with medical professionals:
Health Evaluation: Assess how your weight impacts your health, especially if you have conditions like severe obesity, heart disease, sleep apnea, diabetes, and/or hypertension.
Understand Eligibility: Familiarize yourself with the criteria for bariatric surgery, such as BMI levels and previous weight loss attempts.
Mental Health Consideration: Ensure you are mentally prepared for the surgery and the post-surgery lifestyle changes.
Lifestyle Changes Commitment: Be ready to commit to lifelong changes in diet, exercise, and regular health check-ups.
Educate Yourself: Research the types of surgeries, their risks, and post-surgery life. If you have friends, family, or coworkers who have had the surgery, they can provide information about their experiences as well.
Professional Consultation: Discuss with a bariatric surgeon and possibly seek a second opinion for a comprehensive understanding.
Dietary Counseling: Talk to a dietitian or nutritionist about the necessary nutritional changes post-surgery.
Support System Involvement: Include family and friends in your decision-making process for support.
Financial and Practical Planning: Consider the costs, insurance coverage, recovery time, and other practical aspects of the surgery.
Importance of Medical Consultation:
Expert Guidance and Health Evaluation: Medical professionals provide personalized advice and perform health evaluations to determine suitability for surgery.
Psychological Assessment: They assess mental readiness and suggest necessary support.
Post-Surgery Planning: They guide on diet, exercise, and follow-up care.
Risk Understanding: Doctors help in understanding and managing potential risks.
Understanding the risks and benefits of bariatric surgery is vital for anyone considering this significant medical procedure.
Health Benefits: The surgery can lead to substantial weight loss and improvement in related health conditions, enhancing life quality.
Awareness of Risks: It's crucial to be aware of potential risks, including surgical complications, nutritional deficiencies, and the need for long-term lifestyle changes.
Psychological and Lifestyle Considerations: Understanding the mental health impacts and preparing for a complete lifestyle overhaul post-surgery is essential.
Seeking Professional Advice: Consult with healthcare specialists to receive a personalized assessment and comprehensive understanding of what the surgery entails.
Informed Decision-Making: Reflect on personal health goals, readiness for lifestyle changes, and the overall impact of the surgery on your life.
Consideration of All Aspects: Evaluate the physical, emotional, and financial aspects thoroughly before making a decision.
The decision to undergo bariatric surgery should be made after careful deliberation and consultation with medical professionals. It's important to weigh the potential health benefits against the risks and lifestyle changes required. Making an informed decision is crucial for achieving the best outcomes from the surgery.
Services Offered
Contact Us
By providing my phone number, I agree to receive text messages from the business. (No mobile information will be shared with third parties/affiliates for marketing/promotional purposes)
We will do our best to contact you within a few business days. If you need immediate assistance, please contact 904-296-4141. If you are experiencing a medical emergency, please call 911.
.
Paul D. Bailey, III, MD
SERVICES
OFFICE HOURS
Monday: 8:30 AM–4:30 PM
Tuesday: 8:30 AM–4:30 PM
Wednesday: 8:30 AM–4:30 PM
Thursday: 8:30 AM-4:30 PM
Friday: 8:30 AM–12:30 PM
Saturday and Sunday-Closed
Disclaimer: This website does not provide medical advice. This website including but not limited to text, graphics, and other materials contained on the website are for informational purposes only. No material on the site is intended to be a substitute for professional medical advice, diagnosis, and/or treatment. Always seek the advice of your treating physician or other qualified provider with any questions you have related to your care or condition. Do not delay care or disregard medical treatment due to any content housed on this website.
**Weight-loss results may vary for each individual, and specific results are not guaranteed.